Abstract
Introduction: The presence of hetero- (sickle trait) or homozygous (sickle disease) hemoglobin S gene is associated with increased risk of venous thromboembolism (VTE). However, sickle disease patients in particular are relatively young, lack common comorbid conditions that would qualify them for inpatient VTE prophylaxis (VTEP) and there are limited published data on trends of VTEP use in these populations.
Methods: This was a retrospective analysis of all hospitalizations of sickle trait or disease adult medical patients occurring between January 2013 and December 2018 at three hospitals in Southeast Michigan, USA. Admissions for bleeding or thrombosis, requirement of intensive care stay or surgery, those occurring within 45 days of orthopedic surgery, as well as all patients already on anticoagulation or with known hypercoagulable states were excluded. Hospitalized controls were matched for race, age, sex and length of stay. Trends of VTEP use and predictive patient factors over multiple admissions were modeled using generalized estimating equations.
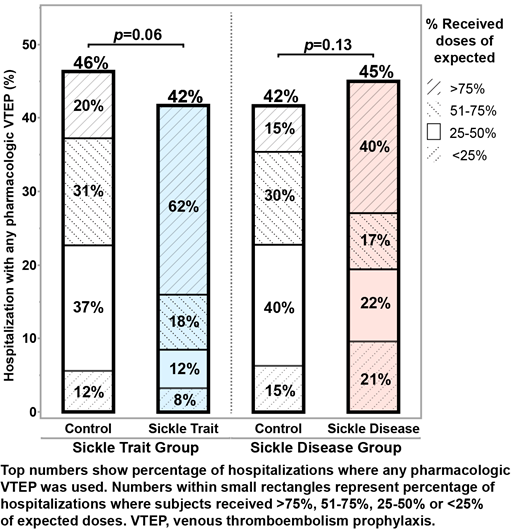
Results: There were 803 sickle trait (525 patients; mean age 43 ± 19; 85% female) and 1020 sickle disease admissions (262 patients; mean age 34 ± 13; 57% female); all patients were Black. The percentage of hospitalizations in which subjects were offered any VTEP was similar to that of controls in both groups of interest (Figure); however, there were more encounters in which patients received greater than 50% of expected VTEP doses in the sickle trait (80% vs 51%; p<0.01) and in the sickle disease group (57% vs 45%; p<0.01). In multivariate analysis, compared to controls, odds of being offered VTEP were similar with sickle trait genotype (adjusted odds ratio [aOR] 0.78; p=0.15), but were higher with sickle disease genotype (aOR 1.45; p=0.02). Increasing age and longer hospital stay were also positive predictors. Within the sickle disease hospitalizations, odds of VTEP use showed significant variability with treatment site (aOR 1.87; p<0.01), whereas comorbid conditions, including a history of VTE prior to admission, or hemoglobin measurement and platelet count on admission did not predict VTEP use. By contrast, in exploring sickle trait admissions, there was no impact of treatment site, but obesity (aOR 1.83; p<0.01), tobacco abuse (aOR 1.64; p=0.03), heart failure (aOR 2.17; p=0.01), prior VTE (aOR 2.22; p=0.07), as well as higher admission hemoglobin (aOR 1.18 per 1 g/dL increase; p<0.01) and platelet count (aOR 1.01 per 10 3 increase; p=0.03) raised the odds of VTEP being offered.
Conclusions: VTEP is underused in sickle trait and disease patients. There may be a trend towards offering more VTEP in sickle disease, but not in sickle trait, where the decision is driven by comorbid conditions rather than hemoglobin genotype. Patient refusal does not appear to play a major role, but the finding of significant inter-center variability suggests provider education may result in improved use as hemoglobin genotype is currently not part of risk stratification tools that help clinicians decide on inpatient VTEP.
No relevant conflicts of interest to declare.